Introduction
Navigating the intricacies of tracheostomy and ventilator training is vital for medical professionals who desire to give ideal take care of clients needing respiratory system support. As healthcare remains to progress, understanding the nuances of air passage administration and air flow has never ever been more crucial. This write-up intends to provide best techniques, understandings, and detailed standards for clinicians involved in tracheostomy and ventilator training.
Understanding Tracheostomy and Ventilator Support
What is a Tracheostomy?
A tracheostomy is a medical treatment that entails developing an opening in the neck to place a tube right into the windpipe (throat). This intervention is often necessary when a person can not take a breath sufficiently due to different conditions, such as severe respiratory system distress, air passage blockage, or prolonged mechanical ventilation requirements.
What is Ventilator Support?
Ventilator assistance refers to the use of equipments that aid or replace spontaneous breathing. It's critical in managing clients with respiratory system failure where standard breathing approaches are insufficient.
Types of Ventilators
Invasive Ventilators: These require intubation or a tracheostomy. Non-invasive Ventilators: These typically utilize masks or nasal devices.Navigating Tracheostomy and Ventilator Training: Ideal Practices for Clinicians
Importance of Comprehensive Training Programs
Clinicians should take part in complete training programs focusing on both tracheostomy treatment and ventilator training ventilator management. Such training courses not only boost medical abilities however likewise foster self-confidence in emergency situations.

Basic Ventilator Program: What to Expect
A standard ventilator training course covers fundamental principles consisting of:

- Understanding different settings of ventilation Adjusting ventilator settings based upon individual needs Recognizing alarm signals
These facets permit medical professionals to react properly throughout crucial care scenarios.
Essential Components of Ventilation Training Courses
Curriculum Summary for Ventilation Training Courses
The ideal educational program should include:
- Anatomy pertinent to air passage management Pathophysiology underlying breathing failure Practical sessions utilizing simulation models
This comprehensive approach ensures that registered nurses are fully equipped with both theoretical understanding and functional expertise.
Ventilator Training for Nurses: Secret Aspects
Nurses play an integral function in managing people on ventilators. Their training must stress:
- Monitoring patient response Troubleshooting typical issues Collaborating with respiratory therapists
Such training ensures alternative care for people requiring advanced air passage management.
Advanced Air passage Monitoring Techniques
Airway Administration Strategies
Effective airway management encompasses various approaches suited to specific patient demands:
Bag-Valve-Mask (BVM) Ventilation: Vital throughout initial resuscitation. Endotracheal Intubation: Made use of when long term air flow is anticipated. Tracheostomy Care: Vital for long-lasting ventilation patients.Each method requires certain skills and understanding, making continuous education and learning vital.
Key Considerations in Tracheostomy Care
Indications for Tracheostomy Placement
Tracheostomies may be indicated when:
- Prolonged mechanical air flow is required. Upper air passage blockage occurs. Patients require a stable airway due to neuromuscular disorders.
Understanding these indications assists medical professionals make informed decisions pertaining to treatment timing.
Post-Tracheostomy Treatment Protocols
After placement, watchful monitoring is crucial. Key protocols include:
Regular suctioning Humidification of inspired air Ensuring tube patencyThese steps significantly minimize issues such as infections or blockages.
Ventilator Settings and Patient Monitoring
Understanding Ventilator Modes and Settings
Clinicians need to excel in changing ventilator settings based upon the complying with criteria:
- Tidal Volume (TELEVISION) Respiratory Rate (RR) Positive End Expiratory Pressure (PEEP)
Each setting plays a considerable duty in enhancing client outcomes during mechanical ventilation.
Monitoring Person Action to Air Flow Support
It's essential to continually assess client action through:
Arterial blood gas evaluation Pulse oximetry Clinical indicators such as frustration or sleepinessProper monitoring can cause prompt interventions, improving overall health care outcomes.
The Function of NDIS in Ventilation Training Courses
NDIS Ventilation Course Overview
The National Special needs Insurance coverage Plan (NDIS) offers specialized courses focused on enhancing medical professional skills in handling people requiring lasting ventilation support.
Benefits of NDIS Ventilation Training Programs
Engaging with NDIS-approved programs uses benefits such as:
Tailored content resolving one-of-a-kind patient needs. Practical workshops emphasizing hands-on learning. Networking opportunities with knowledgeable specialists within the field.These features make sure that medical professionals are well-prepared for real-world challenges they may face when taking care of patients needing complex ventilation support.
Collaborative Approach in Air passage Administration and Ventilation Care
Interdisciplinary Synergy Importance
A collaborative method involving multiple disciplines-- doctors, registered nurses, respiratory therapists-- makes sure extensive treatment distribution for people requiring sophisticated airway administration and ventilation support.
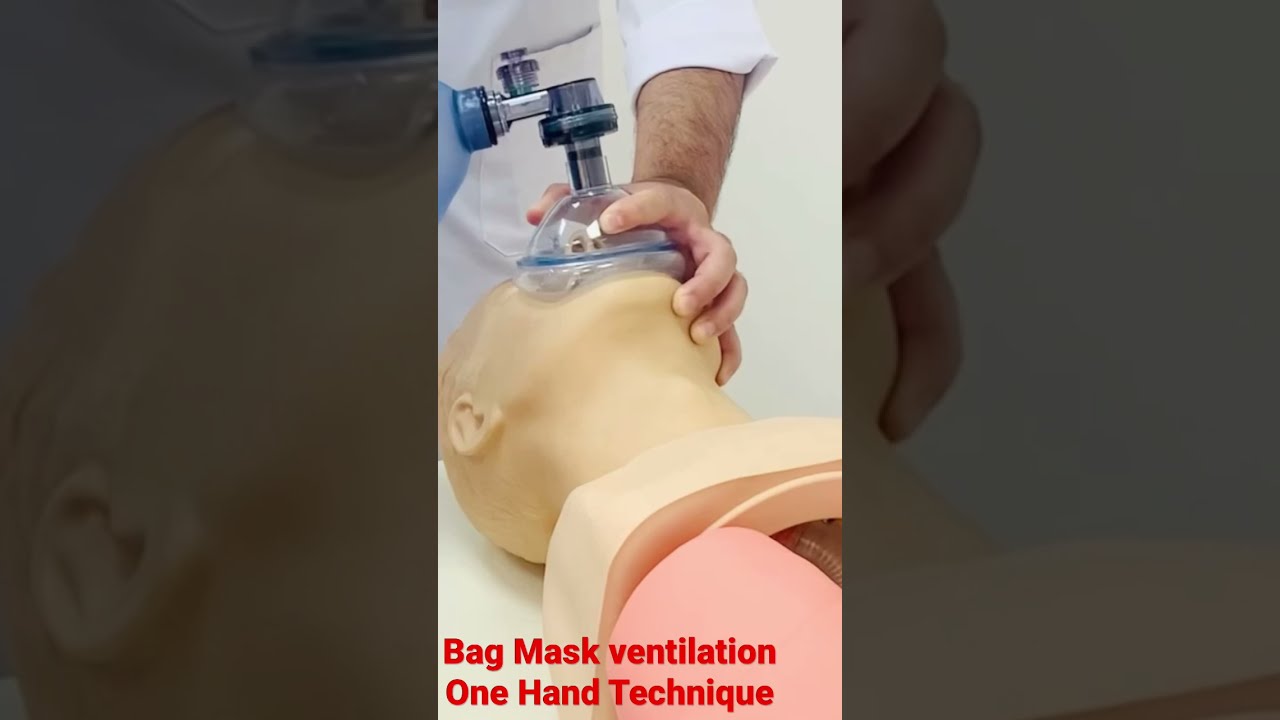
Table 1: Duties of Various Team Members
|Occupation|Function Summary|| --------------------------|-----------------------------------------|| Physician|Diagnostic evaluation & & therapy strategy|| Registered nurse|Client monitoring & & straight treatment|| Respiratory Therapist|Equipment administration & & troubleshooting|
This teamwork boosts interaction, leading to much better patient results while cultivating an environment where constant discovering thrives.
Challenges Dealt with by Clinicians During Tracheostomy and Ventilator Management
Common Challenges
Inconsistent adherence to protocols. Lack of familiarity with devices adjustments. Difficulty identifying problems early on.Recognizing these obstacles enables establishments to carry out targeted educational programs attending to spaces in knowledge or method amongst medical professionals associated with tracheostomy and ventilator care.
FAQ Section
1. What qualifications do I require for basic ventilator training?
To enlist in basic ventilator training courses, it's usually suggested that participants have foundational knowledge in nursing or respiratory system treatment along with scientific experience dealing with people needing respiratory system support.
2. Exactly how frequently should clinicians take part in refresher courses?
Regular correspondence course are advisable every 1-- 2 years; this makes certain that medical professionals continue to be updated on the current practices, technologies, and protocols connected to respiratory tract management.
3. What specific abilities are educated during ventilator training?
Ventilator training gears up individuals with skills such as changing settings based on scientific judgment, identifying alarm system signals from equipment, and executing routine maintenance look at ventilators.
4. Exist any dangers associated with tracheostomy procedures?
Yes, possible dangers consist of bleeding, infection at the incision site, unintended decannulation (elimination of the tube), or injury to surrounding structures.
5. Can non-invasive approaches replace invasive ventilation entirely?
While non-invasive techniques can be effective for sure conditions like COPD exacerbations, invasive techniques stay critical for extreme instances where prompt control over air movement is necessary.
6. How does one evaluate if a patient calls for transitioning from intrusive to non-invasive support?
Clinical standards include enhancement in gas exchange metrics (e.g., reduced carbon dioxide degrees), reduced need for sedation, capability to follow commands indicating neurological status improvement.
Conclusion
Navigating tracheostomy and ventilator training offers both challenges and opportunities for development amongst health care experts committed to boosting client results within this critical location of medication. By embracing constant education with specialized programs such as fundamental ventilator programs or NDIS-approved programs while promoting synergy across techniques boosts our collective capacity-- inevitably connecting gaps Click here for info between understanding deficits experienced during real-time clinical technique experiences encountered daily by frontline workers today!
In summary, cultivating proficiency with structured training not only prepares clinicians but additionally uplifts their self-confidence levels when providing top quality care focused on promoting far better healing paths within vulnerable populaces who depend heavily upon these complex systems designed specifically tailored towards sustaining life itself!